Breadcrumb

What can the UN do to support India through its deadly COVID-19 surge?

'We gave the virus a chance'
Dr. Roderico H. Ofrin, WHO representative to India: It is important to remember that, by early February of this year, the economy and social activities reopened. We also saw that people were not behaving in a way that was appropriate to slowing COVID-19, and I think that's why we are where we are. There are many reasons, but basically, we gave the virus a chance to keep transmitting.
Dr. Yasmin Ali Haque, UNICEF representative to India: In 2020 we were working closely with the Indian Government on spreading health messaging and preventing infections. Life began getting back to normal this year, and this is when the second wave hit.
An overwhelming wave
Dr. Ofrin: The way the virus has spread is similar to what we’ve seen in Europe or the US, but the scale is very different. The density of the population is probably also a factor, and we’ve seen that the spikes are acute in metropolitan areas. In the weeks when the cases were rising, the system was able to absorb patients, and extra beds were also being made available last year. So, it’s a scale issue: the scale of the surge and the scale of the response.
This virus is adapting so fast, that no model has been able to predict how it will spread. We have to be ahead of the game: it’s a cycle of preparedness, readiness, response and recovery. You can’t stop.
However, we do know how to deal with it: consistent testing, contact tracing, active case finding, early treatment, and proper treatment. People need to observe COVID-appropriate behaviours, like the 3W's – Wear a mask, Wash your hands, Watch your distance – and vaccinate. This is the full arsenal of ammunition to fight the virus. it is now a matter of using these tools consistently, and at scale.
Listen below to our full audio interview with Dr. Ofrin:
All hands on deck
Dr. Ali Haque: Right now, we’re focusing on getting essential oxygen equipment. We’re also working on procuring testing machines, and getting COVID vaccines delivered to people. We have a lot of experience vaccinating children, and we’re adapting that experience to anticipate what kind of bottlenecks we’re likely to face, as well as issues of vaccine hesitancy or vaccine eagerness. We have administered close to 160 million doses in about 110 days which is probably the fastest in the world.
The challenge, of course is the numbers, the size of India, the distances and the terrain that sometimes needs to be covered. It's not an easy job, but I believe that, if it’s possible anywhere, it is going to be possible here.

Dr. Ofrin: India is one of the countries that does mass immunisation very, very well. If you look at how things started in the US, they were not used to mass vaccination campaigns. India has a strong tradition and history of vaccinations, and that's why the launch on January 16 went well. However, to achieve herd immunity, we do need to get everyone vaccinated but people also need to behave in ways that are appropriate.
We have been tapping our network of 2600 public health specialists in India, and our experts in the field have been supporting our response: it's all hands on deck for us. Many of our priority areas will continue to surround the maintenance of essential health services. Of course, infection prevention and control is important, but the first priority is filling critical gaps.
Listen below to our full interview with Dr. Ali Haque:
Consequences will last years

Dr. Ali Haque: The consequences of this pandemic will be with us for years. We are already seeing the secondary effects, especially on children and the poorest and most marginalised groups.
In the best-case scenario, we estimate that about 50 per cent of children have access to remote learning. That means that around 150 million children of school-going age do not have access. We are already hearing of stories of an increase in child labour, the early marriage of girls especially and even child trafficking.
We need to address the psychosocial trauma the children are facing now, and to be prepared for the longer term effects. With so many people dying, children are being left without parental care or without caregivers, so there needs to be an investment in fostering and alternative care arrangements for these children.
But I think the way we have seen communities come together, and the extent to which the public has been donating, has been unprecedented. This is going to be crucial if we are to see the investment in critical services that allow children to remain healthy, to thrive, and to recover from the trauma created by this pandemic.

Help from across the UN System
- The UN India team, alongside specialized agencies including the WHO, UNICEF, the UN Development Programme (UNDP) and UN Population Fund (UNFPA) are working closely together to deliver essential equipment in India.
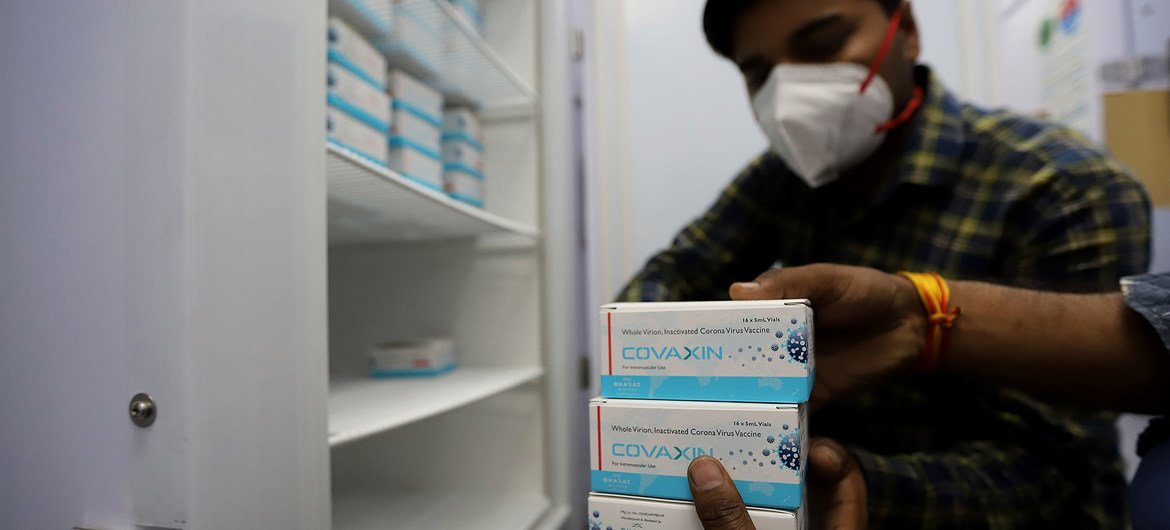
Shortages of oxygen has been linked to many COVID-related deaths during the crisis, with Delhi particularly hard hit. The UN system is providing 10,000 oxygen concentrators, 25 ventilators and over 70 oxygen-generating plants. - Record numbers of tests are being conducted in India, but the current test positivity rate, at 19%, continues to be too high. The UN agencies are supporting the rollout of vaccines, by providing cold chain equipment for the vaccines, with 63 containers of walk-in cold rooms and refrigerators and 200,000 vaccine carriers. WHO and UNICEF also delivered 400,000 machines and 300 kits for testing, with UNICEF further delivering over 60 airport thermal scanners.
- WHO has deployed over 2,600 public health specialists working on other diseases to tackle the pandemic. Across the country, UNICEF and UNDP are also supporting authorities to monitor over 175,000 COVID-19 centres, with over 820 personnel deployed.
